- Home
- ACAMS Certifications
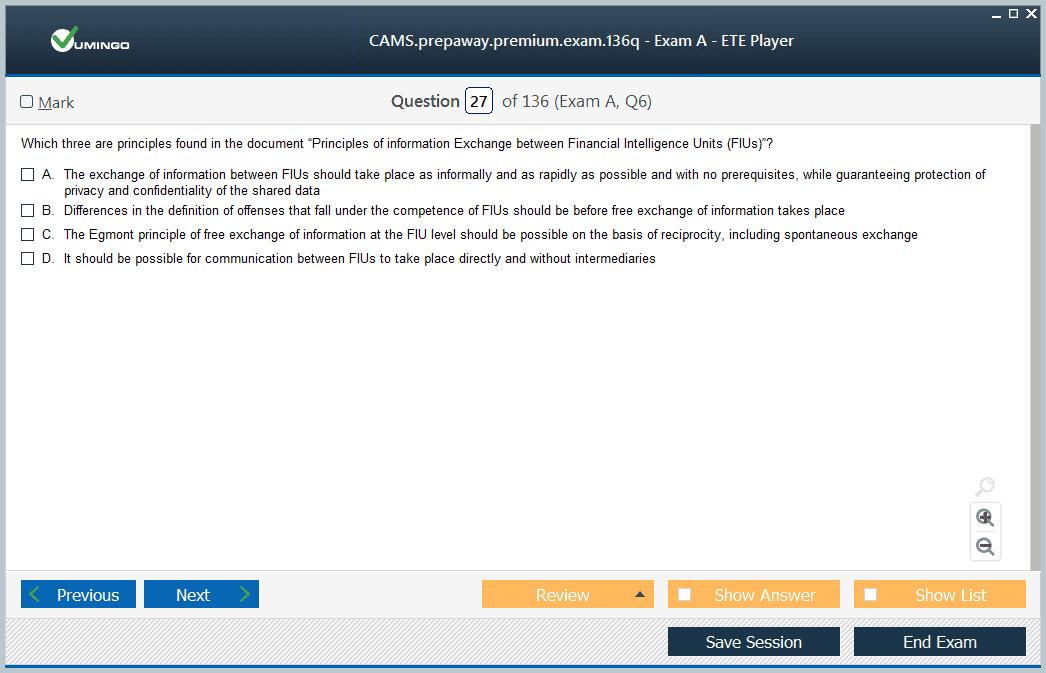
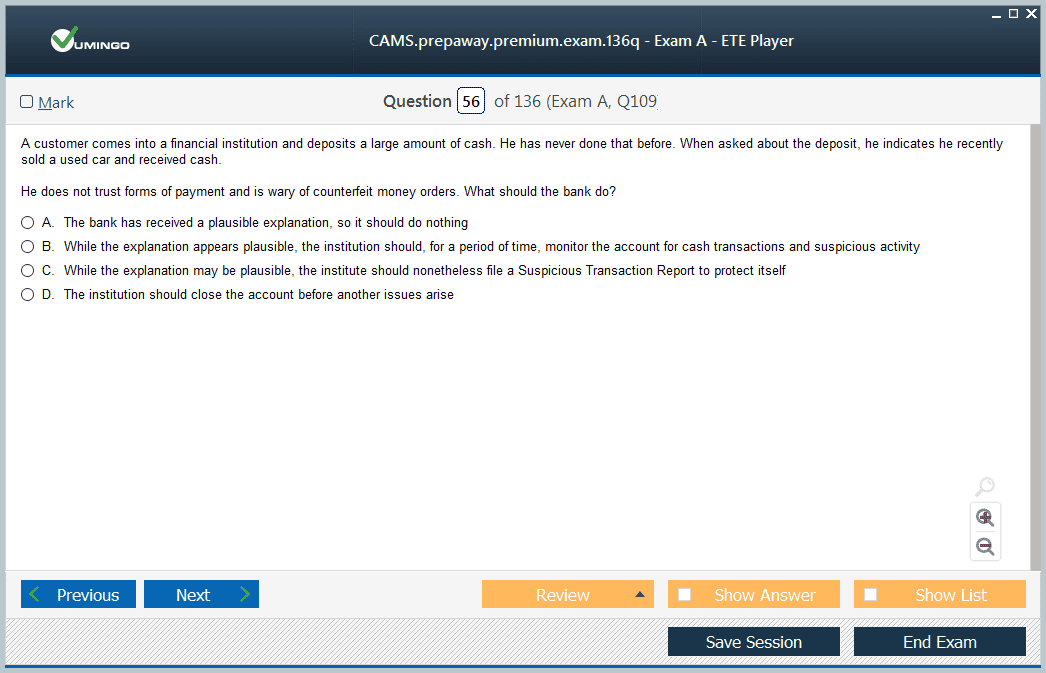
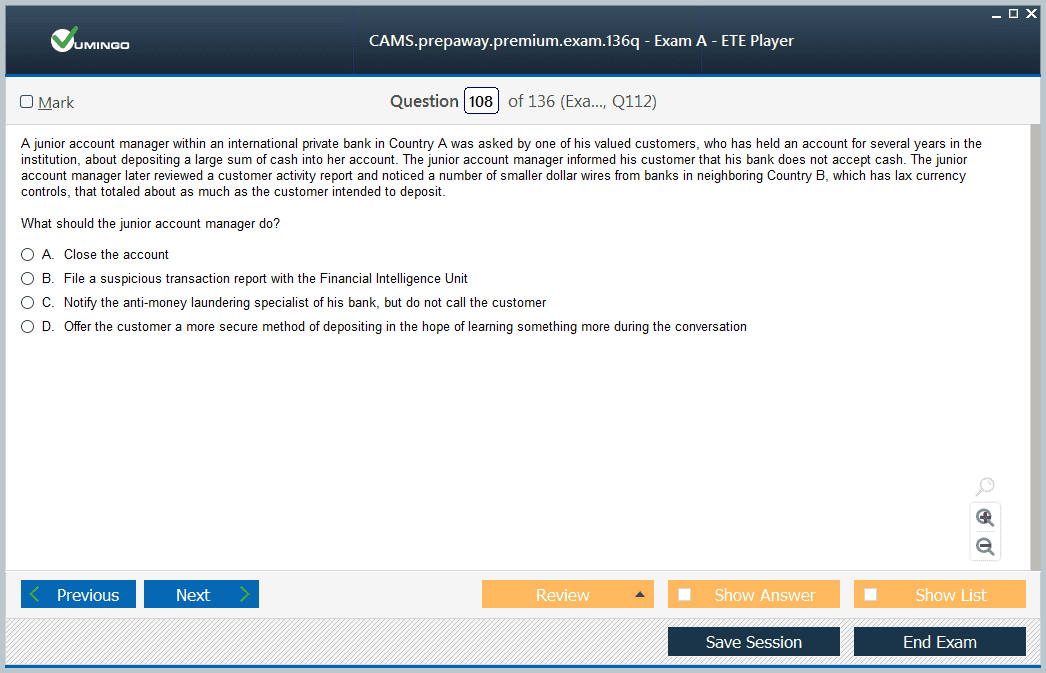
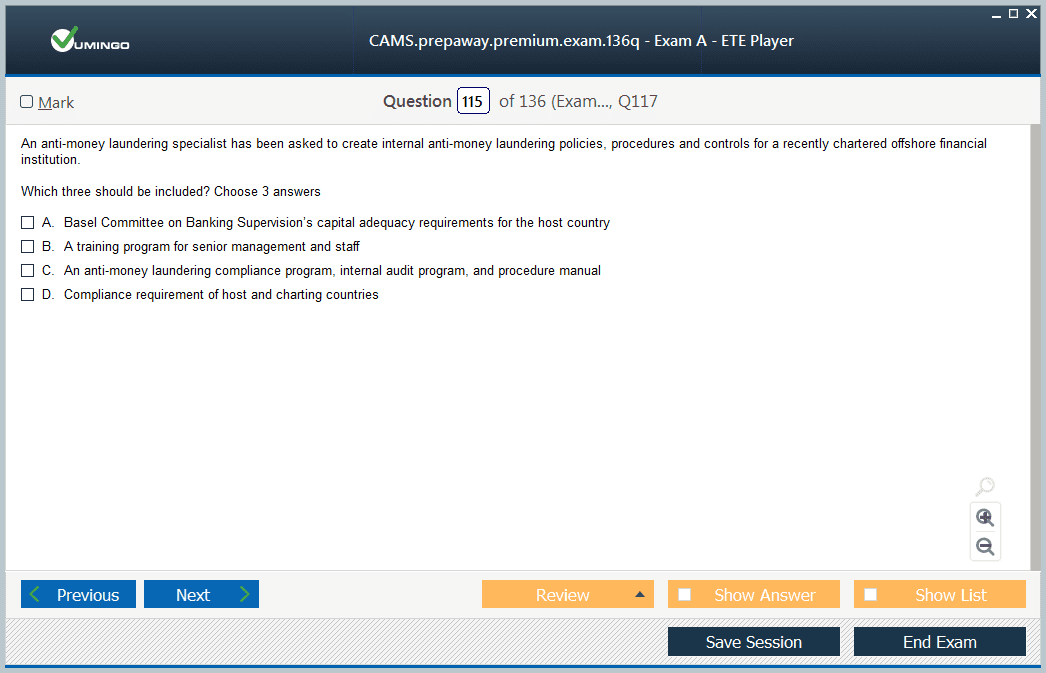
- CAMS Certified Anti-Money Laundering Specialist (the 6th edition) Dumps
Pass ACAMS CAMS Exam in First Attempt Guaranteed!
Get 100% Latest Exam Questions, Accurate & Verified Answers to Pass the Actual Exam!
30 Days Free Updates, Instant Download!

CAMS Premium Bundle
- Premium File 469 Questions & Answers. Last update: Oct 17, 2025
- Training Course 13 Video Lectures
Last Week Results!
Includes question types found on the actual exam such as drag and drop, simulation, type-in and fill-in-the-blank.
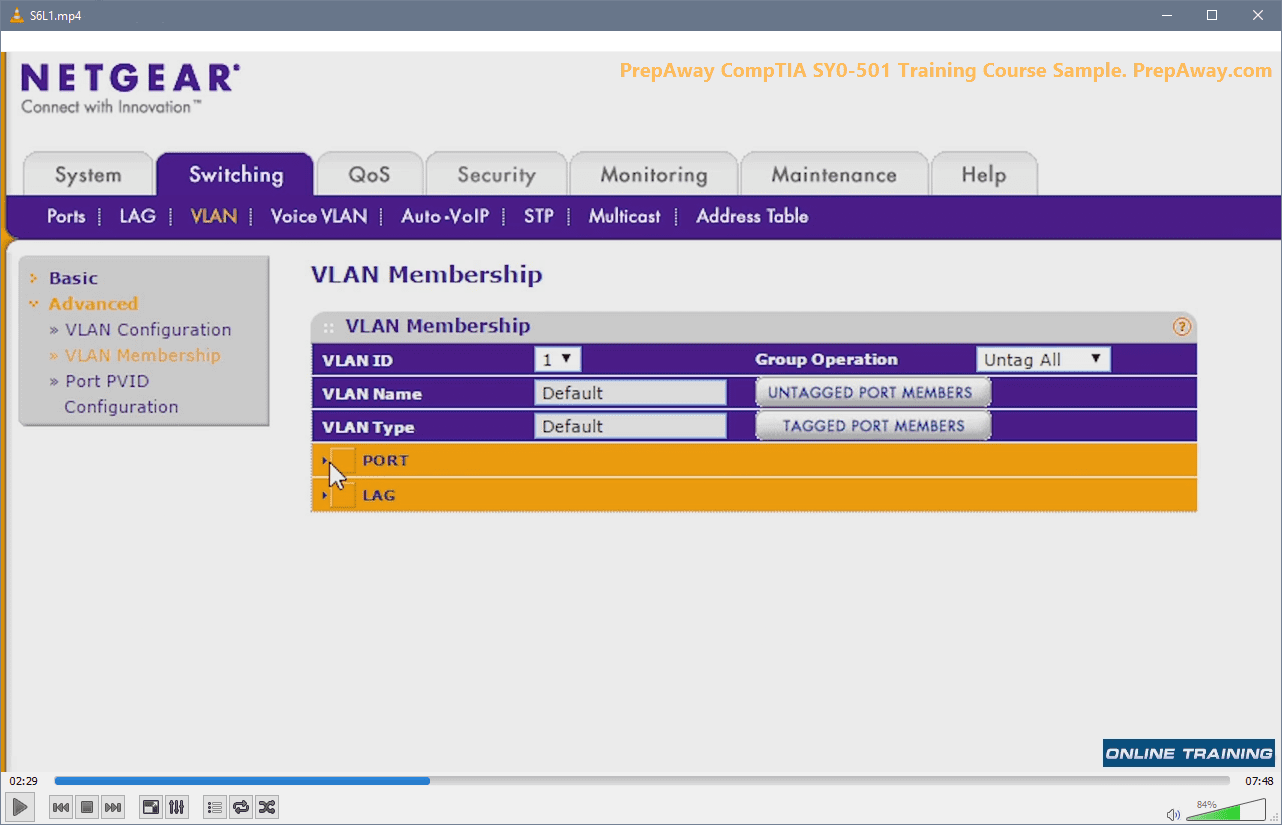
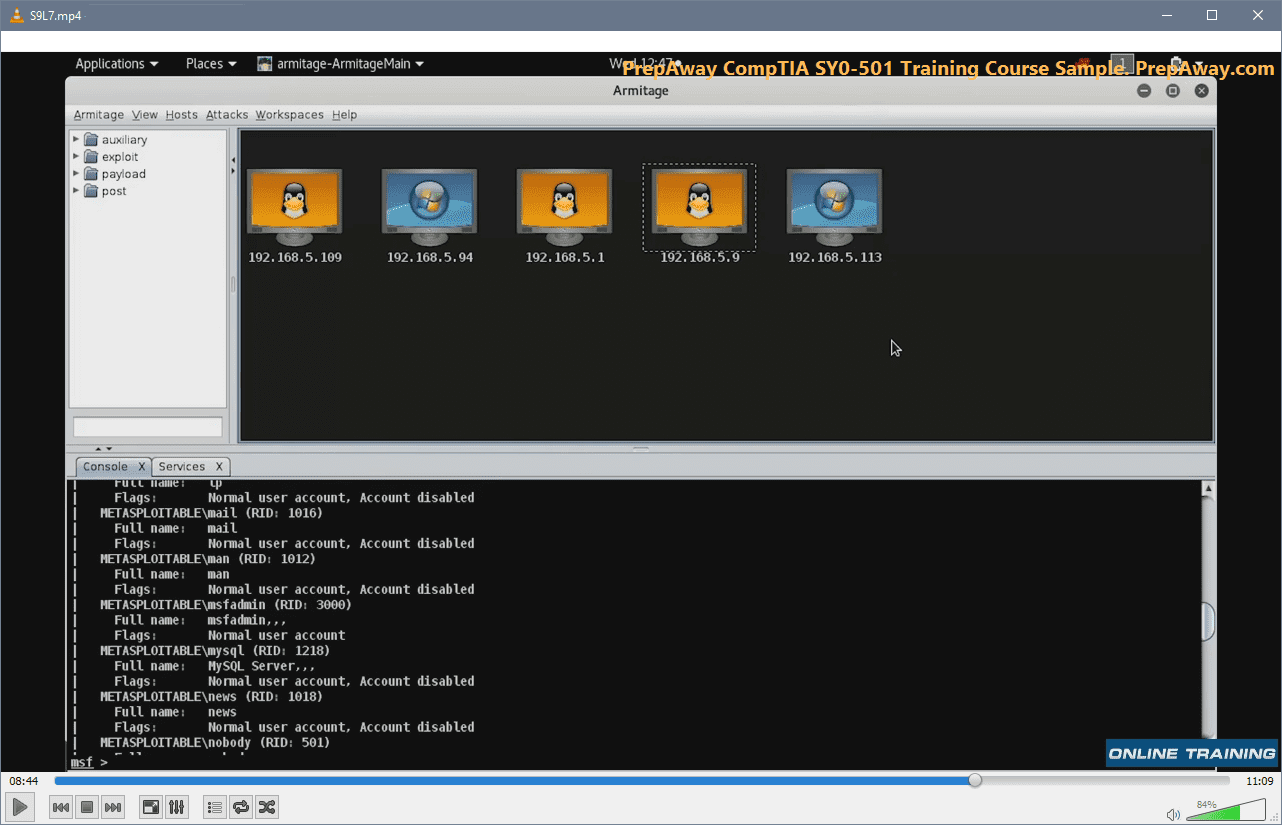
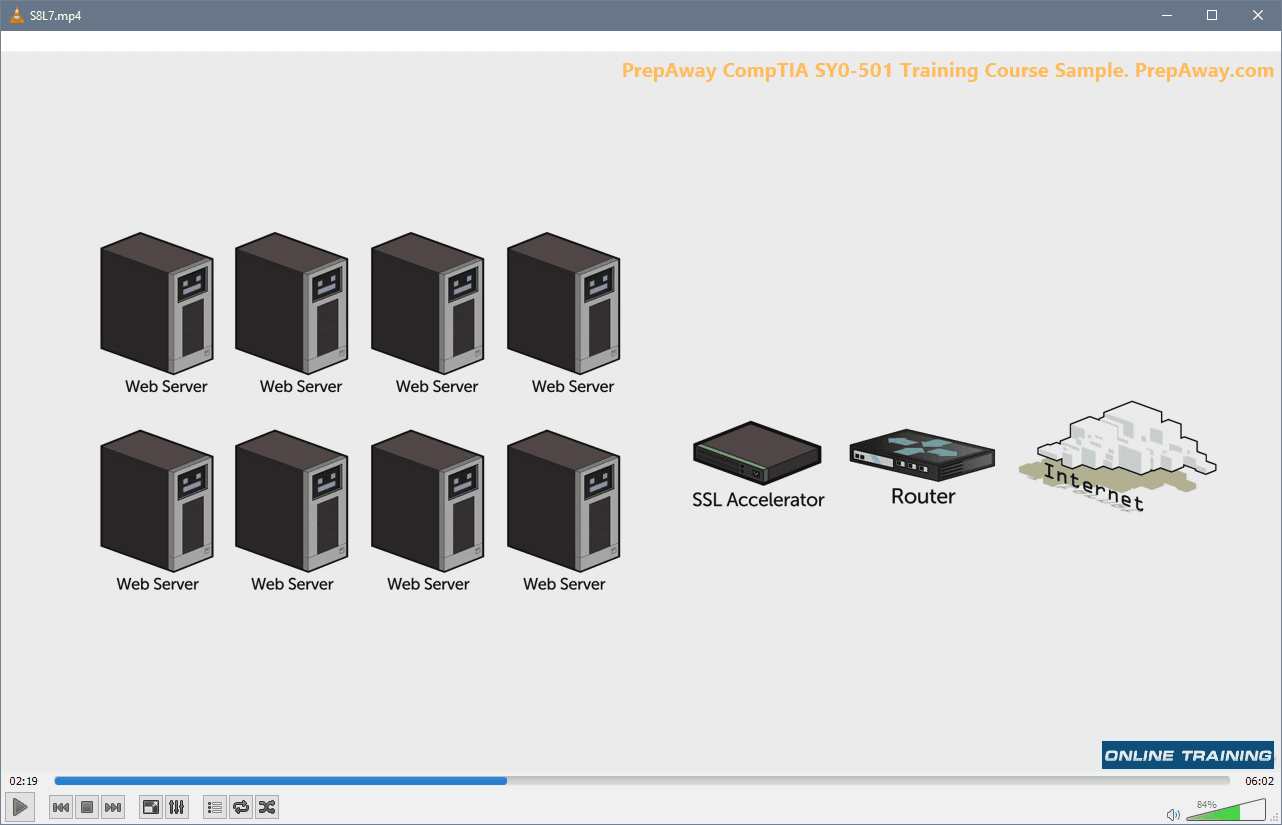
Based on real-life scenarios similar to those encountered in the exam, allowing you to learn by working with real equipment.
All ACAMS CAMS certification exam dumps, study guide, training courses are Prepared by industry experts. PrepAway's ETE files povide the CAMS Certified Anti-Money Laundering Specialist (the 6th edition) practice test questions and answers & exam dumps, study guide and training courses help you study and pass hassle-free!
CAMS and Suicidal Ideation: A Comprehensive Meta-Analysis of Intervention Effectiveness
The Collaborative Assessment and Management of Suicidality, commonly referred to as CAMS, is a therapeutic framework designed specifically to treat individuals experiencing suicidal ideation. The framework evolved from nearly three decades of suicide risk assessment research, beginning in the late 1980s, with its foundational tool, the Suicide Status Form (SSF), guiding all aspects of the intervention. CAMS emphasizes a patient-centered approach in which clinicians collaborate closely with patients to understand the underlying drivers of suicidal thoughts. These drivers, which may include relational stress, trauma, or self-directed negative beliefs, are targeted directly in therapy to achieve meaningful clinical outcomes such as reduced suicidal ideation, decreased symptom distress, and increased hope. The CAMS framework aims to transform the patient’s relationship with suicide, equipping them with alternative coping strategies while promoting engagement in life-affirming goals.
In the summer of 2020, a rigorous meta-analysis of CAMS clinical trials was undertaken by Dr. Joshua Swift, an Associate Professor of clinical psychology at Idaho State University, along with two graduate students. This meta-analysis was designed to synthesize the evidence from multiple clinical trials to assess the effectiveness of CAMS compared to alternative treatment conditions. Importantly, the research team was not composed of suicide treatment researchers, which helped ensure an unbiased perspective in the evaluation. The project identified over 1,000 published and unpublished articles, theses, and dissertations that referred to CAMS or the SSF, eventually narrowing the selection to nine clinical trials that met stringent inclusion criteria. These criteria included the presence of empirical clinical trial data, the inclusion of a comparison control group, and sufficient data to allow statistical analyses across studies.
Methodology of the Meta-Analysis
The methodology of the CAMS meta-analysis followed rigorous, evidence-based procedures for identifying, selecting, and analyzing clinical trials. The research team first conducted a comprehensive search to locate all relevant studies that had implemented CAMS interventions. This search encompassed peer-reviewed journal articles, doctoral dissertations, and other academic sources. Each study was then evaluated according to a set of inclusion criteria designed to ensure methodological rigor. Only studies that included a control condition, such as treatment as usual or alternative therapeutic interventions, were selected for analysis. Additionally, studies had to report sufficient quantitative data to allow calculation of effect sizes for primary clinical outcomes.
Once the nine qualifying studies were selected, the team performed a series of statistical analyses to determine the overall effectiveness of CAMS. The analyses examined weighted average effect sizes across studies, allowing comparison of CAMS to control treatments in terms of reductions in suicidal ideation, symptom distress, hopelessness, and treatment acceptability. The research also explored secondary outcomes, such as suicide attempts, self-harm, and cost-effectiveness, although these findings were preliminary and not statistically significant. Furthermore, moderator analyses were conducted to examine whether patient characteristics, such as racial identity, influenced treatment outcomes. These analyses indicated no significant differences in treatment effects between white and non-white patients, although the majority of clinical samples in the European trials were Caucasian.
Key Findings and Clinical Implications
The results of the meta-analysis demonstrated that CAMS is a highly effective intervention for reducing suicidal ideation and associated psychiatric distress. Compared to control treatments, CAMS produced significant reductions in suicidal thoughts and improved patients’ hope and engagement in treatment. While preliminary analyses of suicide attempts and self-harm were not statistically significant, promising trends were suggesting potential benefits that warrant further investigation. Importantly, none of the studies included in the meta-analysis found that alternative treatments outperformed CAMS in any of the weighted clinical outcomes. The absence of significant allegiance effects or publication bias further strengthens the credibility of these findings, as studies in which the original CAMS developer was directly involved tended to show relatively smaller effect sizes compared to independent trials.
These findings have meaningful implications for clinical practice. CAMS offers a structured yet flexible therapeutic framework that can be implemented in a variety of clinical settings, including outpatient clinics, inpatient units, and crisis intervention services. The intervention is atheoretical, meaning it is not tied to any specific psychotherapeutic orientation, which allows clinicians from different backgrounds to adopt the framework without major modifications. The structured use of the SSF ensures that treatment is suicide-focused, patient-centered, and outcome-oriented, providing a clear roadmap for assessment, intervention, and follow-up care. The framework also facilitates comprehensive clinical documentation, which reflects best practice in suicide risk management and can help reduce liability for practitioners working with high-risk populations.
The Mechanisms Behind CAMS Effectiveness
The effectiveness of CAMS appears to be driven by several key mechanisms. First, the therapeutic alliance between clinician and patient is central to the intervention. By establishing a collaborative relationship, clinicians encourage patients to actively participate in their care and engage with the treatment process. Second, empathy and validation are integral components of CAMS, allowing patients to feel understood and supported during times of extreme distress. Third, the framework directly targets the patient’s suicidal drivers, which are identified using the SSF and addressed through personalized interventions. By focusing on the factors that compel individuals to consider suicide, CAMS provides targeted treatment that addresses the root causes of suicidal ideation rather than simply managing symptoms.
Another critical aspect of CAMS is its ability to change the patient’s relationship with suicide. Patients are encouraged to explore alternative coping strategies, recognize the consequences of suicidal behavior, and develop a renewed sense of purpose and meaning in life. This post-suicidal perspective fosters hope and motivates patients to pursue life goals beyond the crisis. Additionally, CAMS emphasizes early intervention for individuals with suicidal thoughts, potentially reducing the risk of escalation to suicide attempts. By treating the larger population of individuals with suicidal ideation, CAMS addresses the broader public health challenge of suicide prevention, complementing treatments like Dialectical Behavior Therapy and suicide-focused Cognitive Behavioral Therapy, which are more effective in preventing suicide attempts among high-risk individuals.
Practical Applications of CAMS in Clinical Settings
The Collaborative Assessment and Management of Suicidality is designed to be highly adaptable to various clinical environments, providing a structured yet flexible approach for managing suicidal patients. CAMS can be implemented in outpatient therapy clinics, inpatient psychiatric units, emergency departments, and crisis intervention settings. Its atheoretical nature allows clinicians trained in diverse psychotherapeutic orientations to apply the framework effectively. The key tool of CAMS, the Suicide Status Form, functions not only as a clinical assessment instrument but also as a treatment planning and tracking tool. This multipurpose role ensures that each patient’s suicidal drivers are identified early, addressed through tailored interventions, and monitored consistently across sessions. By systematically integrating assessment, intervention, and follow-up, CAMS promotes continuity of care and enhances treatment efficacy.
In outpatient settings, CAMS is particularly effective for patients experiencing moderate to severe suicidal ideation who do not require immediate hospitalization. The framework encourages patients to actively participate in identifying and addressing the factors that drive their suicidal thoughts. By engaging the patient in collaborative problem-solving, clinicians foster a sense of agency and ownership in the treatment process. This approach enhances motivation for change and encourages adherence to treatment recommendations. Clinicians can incorporate evidence-based adjunct therapies, such as cognitive processing therapy, dialectical behavior therapy skills, or motivational interviewing techniques, to address co-occurring psychiatric symptoms, including depression, post-traumatic stress disorder, and anxiety, while maintaining a suicide-focused approach.
In inpatient and crisis intervention contexts, CAMS provides a structured method for stabilizing high-risk patients. The SSF guides clinicians through a thorough assessment of suicidal ideation, intent, and drivers, allowing for rapid identification of acute risk factors. By focusing treatment on the specific drivers of suicidal thoughts, CAMS facilitates the development of personalized safety plans and short-term interventions that can prevent escalation to suicide attempts. The framework also supports clinical decision-making regarding hospitalization and discharge planning, helping clinicians balance risk reduction to minimize unnecessary inpatient stays. The structured documentation afforded by the SSF ensures that patient progress is consistently monitored and communicated across multidisciplinary care teams, enhancing collaboration and reducing the likelihood of treatment gaps.
Training Clinicians in CAMS
Effective implementation of CAMS requires thorough training for clinicians to ensure adherence to the framework and maximize patient outcomes. Training programs typically include workshops, didactic instruction, role-playing exercises, and supervised clinical practice. These programs are designed to familiarize clinicians with the SSF, teach techniques for engaging patients in collaborative assessment, and guide clinicians in the identification and treatment of suicidal drivers. Training emphasizes the importance of building a strong therapeutic alliance, maintaining empathy and validation, and fostering hope for the future. Clinicians are also taught strategies for integrating CAMS with other evidence-based interventions when indicated, allowing for a flexible, patient-centered approach.
Research has shown that clinicians who complete CAMS training demonstrate increased competence, confidence, and adherence to evidence-based suicide-focused practices. This has direct implications for patient outcomes, as well-trained clinicians are more likely to accurately assess risk, engage patients in meaningful interventions, and maintain treatment adherence. Training also equips clinicians with the skills to document care effectively, supporting both clinical decision-making and risk management. By standardizing the approach to suicide-focused care, CAMS training ensures that patients receive consistent, high-quality interventions regardless of the clinical setting or the therapist’s theoretical background.
Case Examples Illustrating CAMS Effectiveness
Illustrative case examples highlight the practical benefits of CAMS and provide insight into how the framework operates in real-world settings. One example involves a military service member experiencing combat-related trauma, personal stressors, and suicidal ideation. Using the SSF, the clinician identified the patient’s primary suicidal drivers, which included PTSD symptoms, concerns about family custody, and occupational stress. The CAMS framework guided the therapeutic process, integrating targeted interventions for PTSD, legal consultation to address custody issues, and career planning for civilian life. Throughout nine sessions, the patient reported a significant reduction in suicidal thoughts, improved mood, and increased hope for the future. This case exemplifies how CAMS targets the underlying drivers of suicidal ideation while promoting engagement in life-affirming goals.
Another case involved an adolescent presenting with chronic depressive symptoms and frequent suicidal thoughts. Through collaborative assessment using the SSF, the clinician identified interpersonal conflict, academic stress, and low self-esteem as primary drivers. CAMS sessions focused on developing coping strategies, enhancing problem-solving skills, and fostering supportive social connections. Within several weeks, the adolescent exhibited decreased suicidal ideation, improved symptom management, and stronger engagement in school and social activities. These case examples demonstrate that CAMS can be effectively applied across diverse age groups and clinical presentations, supporting its broad applicability and reinforcing findings from the meta-analysis regarding consistent reductions in suicidal ideation and symptom distress.
Integration with Other Therapeutic Approaches
While CAMS is a standalone framework for suicide-focused care, it can be effectively integrated with other evidence-based psychotherapies. Clinicians often combine CAMS with cognitive-behavioral therapy to address distorted thinking patterns, dialectical behavior therapy to improve emotion regulation, or exposure-based therapies to target trauma-related symptoms. The flexibility of CAMS allows for these integrations without compromising the core focus on suicidal drivers and collaborative treatment planning. By maintaining a suicide-focused lens, CAMS ensures that the patient’s immediate safety and underlying suicidal drivers remain central to all therapeutic interventions.
Integration with adjunct therapies also supports the treatment of comorbid conditions that may exacerbate suicidal ideation. For example, patients with co-occurring substance use disorders can receive motivational interviewing or contingency management interventions alongside CAMS sessions to address substance-related triggers. Patients with chronic pain or medical illnesses may benefit from incorporating behavioral activation or acceptance-based strategies while maintaining a suicide-focused treatment plan. This adaptability enhances CAMS’s utility across a wide range of clinical populations and treatment settings, allowing clinicians to provide comprehensive care while maintaining fidelity to the evidence-based framework.
Impact on Clinical Outcomes and Patient Engagement
The CAMS meta-analysis revealed that consistent application of the framework produces meaningful improvements in clinical outcomes. Reductions in suicidal ideation were observed across multiple studies, alongside improvements in overall symptom distress and enhanced treatment acceptability. Patients consistently reported feeling understood, validated, and engaged in their care, which facilitated adherence to treatment recommendations. Importantly, CAMS was associated with robust increases in hope and decreases in hopelessness, outcomes that are closely linked to long-term resilience and recovery. These findings highlight that the benefits of CAMS extend beyond immediate symptom reduction to include improvements in patients’ overall psychological well-being and future orientation.
Patient engagement is further enhanced by the collaborative nature of CAMS. By involving patients in the identification of suicidal drivers and the development of treatment strategies, CAMS fosters a sense of agency and empowerment. This collaborative approach encourages active participation in therapy, reinforces motivation for change, and helps patients develop the skills needed to manage future crises independently. Enhanced engagement not only improves clinical outcomes but also strengthens the therapeutic alliance, which is a critical predictor of treatment success across mental health interventions.
Considerations for Diverse Clinical Populations
While the CAMS meta-analysis indicated no significant differences in treatment outcomes based on racial identity, it is important to acknowledge the need for more diverse clinical samples. Most of the European clinical trials primarily included Caucasian participants, and additional research is needed to determine the generalizability of CAMS to populations with different cultural backgrounds, socioeconomic statuses, and language preferences. Clinicians implementing CAMS should consider cultural factors when assessing suicidal drivers and developing interventions. Tailoring treatment approaches to align with patients’ cultural values, beliefs, and lived experiences can enhance engagement, therapeutic alliance, and overall treatment effectiveness.
CAMS is also applicable to individuals across the lifespan, including adolescents, adults, and older adults. The framework’s focus on collaborative assessment and personalized treatment planning allows clinicians to adapt interventions to developmental stages, cognitive abilities, and psychosocial contexts. This flexibility supports the treatment of patients with complex needs, including those experiencing chronic mental illness, trauma histories, or comorbid physical health conditions. By emphasizing individualized care while maintaining a structured, evidence-based approach, CAMS provides a reliable and adaptable method for addressing suicidal ideation in diverse populations.
Long-Term Implementation of CAMS in Clinical Practice
The long-term implementation of the Collaborative Assessment and Management of Suicidality (CAMS) in clinical settings requires careful planning, consistent training, and ongoing supervision. Clinicians who integrate CAMS into routine practice benefit from the structured framework it provides while maintaining flexibility to adapt to individual patient needs. Successful implementation involves establishing organizational support, developing standardized protocols, and ensuring access to training and consultation. Organizations that adopt CAMS as a central component of their suicide prevention strategy report improvements in both patient outcomes and clinician confidence. By embedding the framework into routine care, agencies can create a culture of suicide-focused clinical excellence that emphasizes evidence-based assessment, personalized intervention, and continuous monitoring of patient progress.
Sustained implementation requires clinicians to remain adherent to core principles of CAMS, including the identification of suicidal drivers, collaborative assessment, and continuous outcome monitoring. Supervision and peer consultation are critical in maintaining adherence, particularly for clinicians new to the framework. Regular review of SSF data allows clinicians to track symptom changes, identify emerging risk factors, and adjust treatment plans accordingly. The structured nature of CAMS provides a common language and process across clinicians, which facilitates coordination within multidisciplinary teams and promotes continuity of care. Over time, consistent application of CAMS can contribute to a measurable reduction in suicidal ideation across patient populations and support long-term improvements in overall mental health outcomes.
Cost-Effectiveness and Resource Utilization
CAMS is not only effective in reducing suicidal ideation and associated psychiatric distress but also demonstrates potential advantages in terms of cost-effectiveness and resource utilization. Traditional approaches to suicide prevention, such as repeated inpatient hospitalizations or prolonged psychotropic medication management, often incur substantial costs while yielding limited evidence for reducing suicidal thoughts. In contrast, CAMS emphasizes early, targeted intervention with relatively brief treatment courses, typically six to eight sessions for moderate suicidal ideation. By focusing on the patient’s specific suicidal drivers, CAMS facilitates rapid symptom reduction and decreases the likelihood of acute crises that require intensive resources.
Preliminary analyses from the meta-analysis suggest that CAMS may contribute to more efficient use of clinical resources by preventing escalation to inpatient care, reducing emergency department visits, and improving treatment retention. Additionally, the structured documentation provided by the SSF enhances clinical decision-making and helps organizations manage liability risks, which can further reduce indirect costs associated with malpractice or inadequate record-keeping. While further research is necessary to establish definitive cost-effectiveness metrics, the integration of CAMS into routine practice presents a promising strategy for maximizing therapeutic benefit while optimizing resource allocation.
Advancing Suicide Research Through Meta-Analysis
The CAMS meta-analysis led by Dr. Joshua Swift represents a significant advancement in suicide research, offering an independent, rigorous evaluation of the framework’s effectiveness. By synthesizing data from multiple clinical trials, the meta-analysis provides a high-level overview of the intervention’s impact on suicidal ideation, symptom distress, hopelessness, and treatment acceptability. The findings confirm that CAMS is “well supported” according to the Centers for Disease Control criteria, indicating the highest level of empirical evidence for a clinical intervention targeting suicidal thoughts. Importantly, the meta-analysis mitigated potential bias by including trials in which the original CAMS developer was not involved, ensuring that conclusions reflect objective scientific assessment rather than allegiance effects.
Meta-analytic research also offers the ability to examine moderator effects, identify patterns across diverse populations, and guide future investigations into mechanisms of change. For instance, analyses can explore whether specific patient characteristics, such as age, gender, comorbid conditions, or prior suicide attempts, influence responsiveness to CAMS. Understanding these moderators can help refine treatment protocols, tailor interventions to individual needs, and optimize outcomes. The meta-analysis also establishes a benchmark for comparing CAMS to other evidence-based treatments, such as Dialectical Behavior Therapy or suicide-focused Cognitive Behavioral Therapy, providing clarity on where CAMS offers unique advantages in addressing suicidal ideation.
Future Directions in CAMS Research and Practice
Building on the findings of the meta-analysis, future research can expand our understanding of CAMS by exploring long-term outcomes, mechanisms of change, and population-specific applications. Longitudinal studies that follow patients after CAMS treatment are essential for assessing the durability of symptom reduction, sustained improvements in hope and life engagement, and the prevention of suicide attempts. Investigations into the specific mechanisms by which CAMS reduces suicidal ideation, such as changes in problem-solving skills, emotion regulation, or cognitive reappraisal, can inform enhancements to the framework and support the development of adjunct interventions.
Further research is needed to evaluate the effectiveness of CAMS in diverse populations, including underrepresented racial and ethnic groups, older adults, adolescents, and individuals with comorbid physical health conditions. Expanding clinical trials to international settings will provide insight into cultural and systemic factors that may influence treatment outcomes. Additionally, research on the integration of CAMS with digital health tools, telehealth platforms, and stepped-care models could enhance accessibility and broaden the reach of effective suicide-focused care. Evaluating these innovations will be critical for scaling CAMS to meet the needs of large populations experiencing suicidal ideation.
Enhancing Training and Workforce Development
The successful expansion of CAMS requires investment in workforce development and ongoing clinician support. Comprehensive training programs should include didactic instruction, role-playing, supervised practice, and opportunities for continuing education. Experienced CAMS supervisors and consultants can guide clinicians in complex cases, ensuring fidelity to the framework and maintaining high standards of care. Organizations may also consider implementing peer support networks, case review meetings, and structured feedback mechanisms to reinforce best practices. Building a trained and competent workforce capable of delivering CAMS with fidelity is crucial for maximizing patient outcomes and sustaining the long-term impact of the intervention.
Training initiatives should also address barriers to adoption, such as clinician skepticism, time constraints, and competing demands in busy clinical environments. Emphasizing the evidence-based benefits of CAMS, its structured approach, and its relative ease of learning can enhance clinician engagement and confidence. By equipping clinicians with the skills and resources needed to implement CAMS effectively, organizations can foster a culture of evidence-based suicide-focused care that prioritizes patient safety, clinical excellence, and meaningful recovery.
CAMS and the Broader Suicide Prevention Landscape
CAMS occupies a unique position within the broader landscape of suicide prevention. While treatments such as inpatient hospitalization, psychotropic medication, and specialized therapies like DBT target specific populations or acute risk, CAMS addresses a larger population of individuals experiencing suicidal ideation. By focusing on suicidal thoughts rather than solely on attempts or high-risk behaviors, CAMS offers an upstream intervention that can prevent crises before they escalate. This proactive approach aligns with public health goals of reducing the prevalence of suicidal ideation, enhancing patient engagement, and promoting recovery-oriented care.
Integration of CAMS into community-based mental health services, primary care, and crisis intervention programs can extend its reach and impact. Training a wide range of providers in CAMS principles allows for early identification and intervention for individuals at risk, supporting a stepped-care model of suicide prevention. Furthermore, the structured assessment and documentation facilitated by the SSF can inform population-level monitoring, quality improvement initiatives, and policy development. By contributing to both individual patient care and systemic suicide prevention efforts, CAMS represents a scalable, evidence-based solution to a complex public health challenge.
The Role of Hope and Meaning in Recovery
A central feature of CAMS is its emphasis on fostering hope and meaning in the lives of individuals experiencing suicidal ideation. Research demonstrates that hopelessness is a strong predictor of suicide risk, making its reduction a critical therapeutic target. CAMS sessions focus on identifying patient-driven goals, exploring values, and developing actionable plans that create a sense of purpose. This approach not only alleviates suicidal thoughts but also promotes engagement in life-affirming activities and long-term resilience. Patients report feeling more empowered, motivated, and optimistic about their futures after participating in CAMS-guided care, highlighting the importance of psychological and existential dimensions in recovery.
By addressing the emotional, cognitive, and existential components of suicidal ideation, CAMS supports a holistic approach to treatment. Clinicians work with patients to reframe their relationship with suicide, explore alternative coping strategies, and envision a post-suicidal life with purpose and meaning. This transformation extends beyond symptom reduction, fostering long-term psychological growth, adaptive coping, and sustained engagement in life. The meta-analysis findings underscore the robustness of these outcomes, demonstrating that CAMS reliably reduces hopelessness while enhancing hope across diverse patient populations.
Advanced Clinical Strategies in CAMS Implementation
The Collaborative Assessment and Management of Suicidality (CAMS) offers clinicians a robust framework for addressing suicidal ideation while providing flexibility to tailor interventions to individual patient needs. Advanced clinical strategies within CAMS involve not only identifying and treating suicidal drivers but also integrating complementary evidence-based techniques to optimize outcomes. Clinicians are encouraged to maintain a suicide-focused lens while employing adjunct interventions such as cognitive-behavioral techniques, trauma-focused therapies, and emotion regulation strategies. This approach allows for comprehensive care, addressing both the immediate suicidal risk and the broader mental health context in which it occurs.
Clinicians applying advanced strategies begin by conducting a detailed assessment using the Suicide Status Form (SSF). This tool captures the intensity of suicidal thoughts, identifies primary drivers, and documents the patient’s level of distress. Advanced practice involves using this data to create individualized treatment plans that prioritize the most pressing drivers while also considering comorbid conditions and psychosocial factors. Treatment plans may incorporate exposure-based interventions for trauma, problem-solving therapy for situational stressors, or mindfulness techniques to improve emotional regulation. The structured yet flexible nature of CAMS enables clinicians to adjust interventions based on ongoing assessment, ensuring responsiveness to changing patient needs and maintaining alignment with best practices in suicide-focused care.
Another advanced strategy involves leveraging the therapeutic alliance as a central mechanism of change. Research indicates that a strong, collaborative relationship between clinician and patient enhances engagement, adherence, and outcomes. Clinicians practicing CAMS employ empathic listening, validation, and collaborative problem-solving to foster trust and encourage active patient participation. They emphasize transparency in treatment planning and involve patients in setting goals and evaluating progress. This collaborative approach not only reduces suicidal ideation but also empowers patients to develop adaptive coping skills and a renewed sense of agency in their lives.
Case Studies Demonstrating CAMS Efficacy
Real-world case studies provide compelling evidence of CAMS’s effectiveness and illustrate how advanced clinical strategies are applied. One case involves a military veteran experiencing chronic post-traumatic stress disorder (PTSD), anxiety, and suicidal ideation. The patient’s primary suicidal drivers included trauma-related nightmares, loss of social support, and feelings of failure. Using the SSF, the clinician systematically identified these drivers and collaboratively developed a treatment plan that combined CAMS with cognitive processing therapy. The sessions addressed trauma symptoms while maintaining a suicide-focused perspective. The patient also engaged in problem-solving around reintegration into civilian life, including exploring educational opportunities and potential employment. Within several weeks, suicidal ideation decreased significantly, PTSD symptoms improved, and the patient reported renewed hope and engagement in life.
Another case involved an adolescent experiencing severe depressive symptoms, interpersonal conflict, and suicidal thoughts related to academic stress and social isolation. CAMS sessions focused on identifying suicidal drivers, enhancing coping strategies, and fostering supportive connections with family and peers. The clinician integrated cognitive-behavioral strategies to address negative thought patterns and emotion regulation skills to manage distress. Throughout treatment, the adolescent exhibited reduced suicidal ideation, improved mood, and increased participation in school and extracurricular activities. These case examples highlight how CAMS allows clinicians to address multiple dimensions of risk while maintaining a suicide-focused approach, resulting in measurable improvements in both immediate safety and long-term well-being.
Ethical Considerations in CAMS Practice
Ethical practice is central to the delivery of CAMS-guided care. Clinicians must prioritize patient safety, informed consent, confidentiality, and cultural sensitivity throughout the therapeutic process. Suicide-focused interventions require careful attention to risk assessment, documentation, and adherence to professional standards to ensure that patients receive effective, evidence-based care. CAMS provides a structured framework for addressing these ethical considerations, as the SSF facilitates thorough documentation of assessment, treatment planning, and progress monitoring. Clinicians are expected to maintain professional judgment while adapting interventions to the patient’s context, ensuring that treatment decisions align with ethical guidelines and legal requirements.
In addition to traditional ethical considerations, CAMS emphasizes the importance of fostering hope and autonomy. Patients are treated as active collaborators rather than passive recipients of care, supporting their right to participate meaningfully in decision-making. Clinicians are guided to balance the need for safety with respect for patient agency, helping patients develop coping strategies and plan for future crises. Ethical practice in CAMS also involves recognizing the limits of one’s expertise and seeking consultation or referral when patients present with complex or high-risk needs. By integrating structured assessment, collaborative intervention, and ethical vigilance, CAMS ensures that clinicians provide responsible, patient-centered suicide-focused care.
Integration with Healthcare Systems and Multidisciplinary Teams
CAMS is most effective when integrated into broader healthcare systems that support multidisciplinary collaboration. Clinicians applying CAMS often work alongside psychiatrists, social workers, nurses, case managers, and other professionals to address the multifaceted needs of patients at risk for suicide. The SSF serves as a communication tool across team members, providing consistent, up-to-date information about suicidal ideation, drivers, and treatment progress. This integration enhances continuity of care, reduces the risk of treatment gaps, and supports coordinated decision-making regarding hospitalization, outpatient care, and follow-up services.
Multidisciplinary implementation of CAMS also facilitates systemic improvements in suicide prevention. Healthcare organizations can standardize protocols for suicide-focused assessment, documentation, and intervention, ensuring that patients receive evidence-based care across settings. Training programs for staff at all levels, from front-line clinicians to administrative personnel, support the sustainability of CAMS within complex healthcare systems. By embedding CAMS into organizational structures, agencies can create a culture of suicide-focused care, promote adherence to best practices, and improve outcomes for a broad patient population.
Addressing Comorbidities and Complex Cases
Many patients who experience suicidal ideation present with comorbid psychiatric or medical conditions that complicate treatment. CAMS provides a flexible framework for addressing these complexities while maintaining a focus on suicide prevention. For example, patients with co-occurring substance use disorders may require integrated interventions that address both substance-related triggers and suicidal drivers. Patients with chronic medical conditions may benefit from combining CAMS with behavioral health interventions that target pain management, functional limitations, or illness-related stress. The framework’s emphasis on individualized assessment allows clinicians to prioritize interventions based on the most salient risk factors while addressing broader psychosocial needs.
Complex cases may also involve patients experiencing acute crises, multiple co-occurring psychiatric diagnoses, or high levels of environmental stress. CAMS encourages clinicians to implement structured risk assessment, collaborative safety planning, and ongoing monitoring while incorporating adjunct therapies as needed. The framework’s flexibility allows for the sequencing of interventions, targeting immediate safety concerns first and gradually addressing underlying drivers of suicidal ideation. Through systematic application of these strategies, CAMS supports clinicians in managing high-risk patients effectively while promoting recovery and resilience.
Measuring Outcomes and Quality Improvement
Systematic measurement of outcomes is a cornerstone of CAMS implementation. The SSF provides quantitative data on suicidal ideation, symptom distress, hopelessness, and treatment engagement, allowing clinicians to track changes over time. This data not only informs individual treatment decisions but also contributes to organizational quality improvement initiatives. By aggregating SSF data across patients, organizations can identify trends, evaluate the effectiveness of interventions, and refine clinical protocols. Continuous monitoring supports evidence-based practice, accountability, and the demonstration of clinical value to stakeholders.
Outcome measurement also enables the identification of areas for clinician development and supervision. Regular review of treatment outcomes allows supervisors to provide targeted feedback, reinforce adherence to CAMS principles, and address challenges in implementation. This iterative process ensures that clinicians maintain high standards of care, improve treatment fidelity, and maximize patient benefit. By combining structured assessment, outcome measurement, and continuous quality improvement, CAMS provides a comprehensive framework for delivering accountable, effective, and patient-centered suicide-focused care.
The Broader Public Health Impact of CAMS
CAMS has implications beyond individual patient care, contributing to population-level suicide prevention strategies. By targeting suicidal ideation, CAMS addresses a larger population than interventions focused solely on suicide attempts or high-risk behaviors. Early and effective intervention for individuals experiencing suicidal thoughts can prevent escalation to attempts, hospitalizations, or long-term psychiatric morbidity. Integration of CAMS into community mental health programs, primary care, and crisis services supports proactive suicide prevention and aligns with public health goals of reducing the overall prevalence of suicide-related outcomes.
Implementation of CAMS across multiple clinical settings also enables the collection of population-level data on suicidal ideation, treatment engagement, and outcomes. This information can inform policy development, resource allocation, and program evaluation. By demonstrating both clinical efficacy and practical feasibility, CAMS provides a scalable, evidence-based approach to suicide prevention that can be adapted to diverse healthcare systems and community contexts.
Conclusion:
The meta-analysis of CAMS conducted by Dr. Joshua Swift and colleagues confirms the framework’s effectiveness in reducing suicidal ideation, symptom distress, and hopelessness while increasing treatment acceptability and patient engagement. CAMS represents a flexible, evidence-based approach that can be applied across clinical populations, settings, and theoretical orientations. The SSF provides a structured tool for assessment, treatment planning, and outcome measurement, supporting both individual patient care and organizational quality improvement.
Future directions for CAMS include expanding research on diverse populations, exploring long-term outcomes, and investigating the mechanisms underlying treatment effectiveness. Integration with digital health technologies, telehealth platforms, and multidisciplinary care models may enhance accessibility and scalability. Continued emphasis on clinician training, ethical practice, and workforce development will ensure that CAMS maintains fidelity while reaching a growing number of patients at risk for suicide. By combining structured assessment, collaborative intervention, and a focus on hope and meaning, CAMS offers a comprehensive, patient-centered approach to one of the most pressing challenges in mental health today.
ACAMS CAMS practice test questions and answers, training course, study guide are uploaded in ETE Files format by real users. Study and Pass CAMS Certified Anti-Money Laundering Specialist (the 6th edition) certification exam dumps & practice test questions and answers are to help students.
Exam Comments * The most recent comment are on top
Purchase CAMS Exam Training Products Individually
Why customers love us?
What do our customers say?
The resources provided for the ACAMS certification exam were exceptional. The exam dumps and video courses offered clear and concise explanations of each topic. I felt thoroughly prepared for the CAMS test and passed with ease.
Studying for the ACAMS certification exam was a breeze with the comprehensive materials from this site. The detailed study guides and accurate exam dumps helped me understand every concept. I aced the CAMS exam on my first try!
I was impressed with the quality of the CAMS preparation materials for the ACAMS certification exam. The video courses were engaging, and the study guides covered all the essential topics. These resources made a significant difference in my study routine and overall performance. I went into the exam feeling confident and well-prepared.
The CAMS materials for the ACAMS certification exam were invaluable. They provided detailed, concise explanations for each topic, helping me grasp the entire syllabus. After studying with these resources, I was able to tackle the final test questions confidently and successfully.
Thanks to the comprehensive study guides and video courses, I aced the CAMS exam. The exam dumps were spot on and helped me understand the types of questions to expect. The certification exam was much less intimidating thanks to their excellent prep materials. So, I highly recommend their services for anyone preparing for this certification exam.
Achieving my ACAMS certification was a seamless experience. The detailed study guide and practice questions ensured I was fully prepared for CAMS. The customer support was responsive and helpful throughout my journey. Highly recommend their services for anyone preparing for their certification test.
I couldn't be happier with my certification results! The study materials were comprehensive and easy to understand, making my preparation for the CAMS stress-free. Using these resources, I was able to pass my exam on the first attempt. They are a must-have for anyone serious about advancing their career.
The practice exams were incredibly helpful in familiarizing me with the actual test format. I felt confident and well-prepared going into my CAMS certification exam. The support and guidance provided were top-notch. I couldn't have obtained my ACAMS certification without these amazing tools!
The materials provided for the CAMS were comprehensive and very well-structured. The practice tests were particularly useful in building my confidence and understanding the exam format. After using these materials, I felt well-prepared and was able to solve all the questions on the final test with ease. Passing the certification exam was a huge relief! I feel much more competent in my role. Thank you!
The certification prep was excellent. The content was up-to-date and aligned perfectly with the exam requirements. I appreciated the clear explanations and real-world examples that made complex topics easier to grasp. I passed CAMS successfully. It was a game-changer for my career in IT!

I have interested in getting few exam dumps for cams and other exams. Kindly let me know the details along with pricing and money back guarantee
Thanks